
Our Location
Opp. Gulbai Tekra Approach BRTS Stand,
University to Panjrapole Road, Ambavadi,
Ahmedabad, Gujarat 380015
Andrology is sub-speciality of Urology pertaining to male infertility & Erectile dysfunction.
Erectile Dysfunction (Impotence)
Impotence is chronic inability to have an erection rigid enough & that can be sustained for a long enough period to complete sexual intercourse for at-least half of the times sexual inter course takes place.
Impotence is very common condition, can be due to physical or psychological causes.
Physical impotence:
It may result from damage to nerves or blood vessels that control flow of blood to the penis.It may be also caused by problems with hormones which control sexual development & function.Certain medicines & habits like smoking,alcoholism can lead to Impotence.Certain structural disease like Chordee (Curvature of Penis) or peyronie's disease (hard plaque in penis) can interfere in sexual intercourse.
Psychological impotence:
It can be a result of fear,stress,worry,anger or frustration.Often this type of impotence develops from performance anxiety-man's fear that he may not be able to perform well during sexual intercourse.Stress caused by problem on the job,marital problems or financial problems can also cause impotence.Depression due to any cause can lead to impotence.
If erections do not become firm to allow for vaginal penetration, have Impotence. If erctions have the necessary rigidity, but are only firm for brief period, you may have the problem. If your erection loses its strength upon penetration, you probably have the problem.
If any of the above scenarios fit, it may be the time to admit it & consult the specialist.
Erectile dysfunction can occur in man at any age. According to National Institute of Health,5% of men at the age of 40 & approximately 15-25% of men at the age of 65 or above have some degree of erectile dysfunction.
Impotence can also be caused due to diabetes. Overall incidence of impotence in male with diabetes is 2 to 5 times higher than the general male population.

How to diagnose Impotence?
Nature of the impotence:
The first step in the diagnosis is to determine whether the impotence is due to physical or psychological causes.For this the physician, will ask certain set of questions & take detailed history.He will inquire regarding any past illness,surgery,medications etc.
General examination:
Physician will then conduct through general examinations as well as examine the external genitalia to find out the cause.
Laboratory test:
Apart from routine blood & urine tests ask for test to check hormone levels.
Doppler study:
For doppler study of penis to check for blood inflow & out flow from penis.
Treatment overview:
For most men cause of Impotence can now be identified easily.Once identified proper treatment can be recommended to help them return to a satisfactory sex life.
If you have impotence should consult specialist for evaluation & treatment of your problem. Today there are many effective treatment options available to choose from both surgical & non-surgical. In many cases, several of these treatment options may be appropriate. The patient may then choose the treatment method which he feels comfortable.
Following are the few options available for treatment of Impotence your physician may suggest.
Quitting smoking & changing medications:
Certain medications interfere in sexual function. Simply changing the medication may resolve the problem.
Hormonal medications:
Less than 5% of erectile dysfunction cases are caused by irregular levels of sex hormones, such as low levels of testosterone or excess oestrogen.
There are oral medications, injections, gels and spraythat restore this balance.
Counselling
Many times, problem can be resolved by Professional Counselling. Even in Physical causes counselling can reduce the anxiety of patient.
Oral Medications
Multiple medications which help in improving erection are available like Sildenafil (Viagra), Tadalafil etc.These medicines work by increasing Nitro-oxide (Mediators in erection). However, these drugs have interactions with other drugs and should be used with caution in patient with cardiac risk factors.
Vaccum therapy
This treatment enables erection by increasing blood flow to the Penis through negative pressure suction generated by the device used for this treatment. In this way patient, can obtain penile enlargement and rigidity necessary for sexual intercourse.
Injection therapy
One of newest form of treatment involves the self-injection of certain medication into the side of penis. This relatively painless injection produces erection of good quality in about 70-80% of patients.
Surgical treatment
This treatment is generally reserved for those patients whose blood flow has been blocked by an injury to Penis or Pelvic area. For these select candidates, a surgery to correct a blocked artery as a leak in the pelvic veins is an option.
Penile prosthesis
The most common surgical procedure to treat Impotence is penile prosthesis implantation. This treatment involves the surgical placement of a device in to the two sides of the penis, allowing erections as often as desired.These Implantations comes in two terms – an inflatable device and semi rigid rods. This treatment is recommended only after discussing with the Patient all other available options. A Prosthesis is a long team solution, which is offered after careful consideration and Discussion with the Patient.
Surgical treatments for structural diseases
Surgery for correction of curvater of penis (Chordee) by surgery can restore sexual dysfunction. Removal of Plaque in the Penis (Peyronie's Plaque) by Surgery helps in improving sexual dysfunction.
Overall the good news for many men and their partners is that erectile dysfunction can usually be treated safely and effectively. Their impotency no longer needs to remain as disruptive factor in their relationship.
What is Male Infertility?
This means they aren't able to conceive a child even though they've had frequent, unprotected sexual intercourse for a year or longer. In up to half of these couples, male infertility plays a role.
Male infertility is due to low sperm production, abnormal sperm function or blockages that prevent the delivery of sperm. Illnesses, injuries, chronic health problems, lifestyle choices and other factors can play a role in causing male infertility.
Not being able to conceive a child can be stressful and frustrating, but a number of male infertility treatments are available.
About 13 out of 100 couples can't get pregnant with unprotected sex. There are many causes for infertility in men and women. In over a third of infertility cases, the problem is with the man. This is most often due to problems with his sperm production or with sperm delivery.
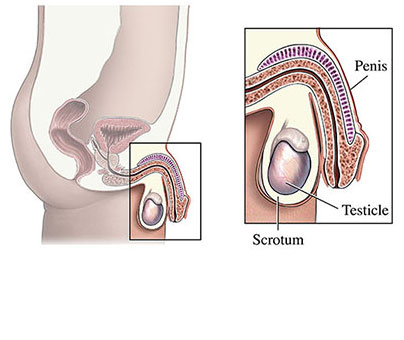
What Happens Under Normal Conditions?
Sperms are produced in testis. During sexual Intercourse, ejaculation normally delivers the sperm into the woman's body.
The male reproductive system produces, stores, and transports sperm. Chemicals in your body called hormones control this. Sperm and male sex hormone (testosterone) are made in the testicles. The testicles are in the scrotum, a sac of skin below the penis. When the sperm leave the testicles, they go into a tube behind each testicle. This tube is called the epididymis.
Just before ejaculation, the sperm go from the epididymis into another set of tubes. These tubes are called the vas deferens. Each vas deferens leads from the epididymis to behind your bladder in the pelvis. There each vas deferens joins the ejaculatory duct from the seminal vesicle. When you ejaculate, the sperm mix with fluid from the prostate and seminal vesicles. This forms semen. Semen then travels through the urethra and out of the penis.
Male fertility depends on your body making normal sperm and delivering them. The sperm go into the female partner's vagina. The sperm travel through her cervix into her uterus to her fallopian tubes. There, if a sperm and egg meet, fertilization happens.
The system only works when genes, hormone levels and environmental conditions are right.
What Causes Male Infertility?
Making mature, healthy sperm that can travel depends on many things. Problems can stop cells from growing into sperm. Problems can keep the sperm from reaching the egg. Even the temperature of the scrotum may affect fertility. These are the main causes of male infertility:
Sperm Disorders
The most common problems are with making and growing sperm. Sperm may:
- not grow fully
- be oddly shaped
- not move the right way
- be made in very low numbers (oligospermia)
- not be produced at all (azoospermia)
Smoking, drinking alcohol, and taking certain medications can lower sperm numbers. Other causes of low sperm numbers include long-term sickness (such as kidney failure), childhood infections (such as mumps), and chromosome or hormone problems (such as low testosterone).
Damage to the reproductive system can cause low or no sperm. About 4 out of every 10 men with total lack of sperm (azoospermia) have an obstruction (blockage). A birth defect or a problem such as an infection can cause a blockage.
Varicoceles
Varicoceles are swollen veins in the scrotum. They're found in 16 out of 100 of all men. They are more common in infertile men (40 out of 100). They harm sperm growth by blocking proper blood drainage. The testicles are then too warm for making sperm. This can cause low sperm numbers.
Retrograde ejaculation
Retrograde ejaculation is when semen goes backwards in the bladder. They go into your bladder instead of coming out the penis. This happens when nerves and muscles in your bladder don't close during orgasm (climax). Semen may have normal sperm, but the semen cannot reach the vagina.
Retrograde ejaculation can be caused by surgery, medications or health problems of the nervous system. Signs are cloudy urine after ejaculation and less fluid or "dry" ejaculation.
Immunologic Infertility
Sometimes a man's body makes antibodies that attack his own sperm. Antibodies are most often made because of injury, surgery or infection. They keep sperm from moving and working normally. We don't know yet exactly how antibodies lower fertility. We do know they can make it hard for sperm to swim to the fallopian tube and enter an egg. This is not a common cause of male infertility.
Obstruction
Sometimes sperm can be blocked. Repeated infections, surgery (such as vasectomy), swelling or developmental defects can cause blockage. Any part of the male reproductive tract can be blocked. With a blockage, sperm from the testicles can't leave the body during ejaculation.
Hormones
Hormones made by the pituitary gland tell the testicles to make sperm. Very low hormone levels cause poor sperm growth.
Chromosomes
Sperm carry half of the DNA to the egg. Changes in the number and structure of chromosomes can affect fertility. For example, the male Y chromosome may be missing parts.
Medication
Certain medications can change sperm production, function and delivery. These medications are most often given to treat health problems like:
- arthritis
- depression
- digestive problems
- infections
- high blood pressure
- cancer
How is Male Infertility Diagnosed?
Causes of male fertility can be hard to diagnose. The problems are most often with sperm production or delivery. Diagnosis starts with a full history and physical exam. Your health care provider may also want to do blood work and semen tests.
History and Physical Exam
Your health care provider will take your health and surgical histories. Doctor will want to know about anything that might lower your fertility. These might include defects in your reproductive system, low hormone levels, sickness or accidents.
Doctor will ask about childhood illnesses, current health problems, or medications that might harm sperm production. Such things as mumps, diabetes and steroids may affect fertility. Doctor will also ask about your use of alcohol, tobacco, marijuana and other recreational drugs. He or she will ask if you've been exposed to ionizing radiation, heavy metals or pesticides. Heavy metals are an exposure issue (e.g. mercury, lead arsenic). All of these can affect fertility.
Doctor will ask about sexual history. He or she will want to know about you and your partner's efforts to get pregnant. For example, your healthcare provider may ask if you've had trouble with erections.
The physical examination will look for problems in your penis, epididymis, vas deferens, and testicles. Your doctor will look for varicoceles. They can be found easily with a physical exam.
Semen Analysis
Semen analysis is a routine lab test. It helps show the cause of male infertility. The test is most often done twice. Semen is collected by having you masturbate or intercourse into a sterile cup. The semen sample is studied. It can be checked for things that help or hurt conception (fertilization).
Your health care provider will study your sperm volume, count, concentration, movement ("motility"), and structure. The quality of your sperm tells much about your ability to conceive (start a pregnancy). For instance, semen is normal if it turns from a pearly gel into a liquid within 20 minutes. If not, there may be a problem with the seminal vesicles, your male sex glands. Lack of fructose (sugar) in a sperm-free sample may mean there are no seminal vesicles. Or it may mean there is a blocked ejaculatory duct.
Even if the semen test shows low sperm numbers or no sperm, it may not mean you are permanently infertile. It may just show there's a problem with the growth or delivery of sperm. More test may be needed.
Transrectal Ultrasound
Your health care provider may ask a transrectal ultrasound. Ultrasound uses sound waves bouncing off an organ to get a picture of the organ. A probe is placed in the rectum. It beams sound waves to the nearby ejaculatory ducts. The health care provider can see if structures such as the ejaculatory duct or seminal vesicles are poorly formed or blocked.
Testicular Biopsy
If a semen test shows a very low number of sperm or no sperm you may need a testicular biopsy. This test can be done in an operating room with general or local anesthesia. A small cut is made in the scrotum. It can also be done in a clinic using, a needle through the numbed scrotal skin. In either case, a small piece of tissue from each testicle is removed and studied under a microscope. The biopsy serves 2 purposes. It helps find the cause of infertility. And it can collect sperm for use in assisted reproduction.
Hormonal Profile
The health care provider may check your hormones. This is to learn how well your testicles make sperm. It can also rule out major health problems. For example, follicle-stimulating hormone (FSH) is the pituitary hormone that tells the testicles to make sperm. High levels may mean your pituitary gland is trying to get the testicles to make sperm, but they won't.
How is Male Infertility Treated?
Treatment depends on what's causing infertility. Many problems can be fixed with drugs or surgery. This would allow conception through normal way.
The treatments below are broken into 3 categories:
- Non-surgical therapy for Male Infertility
- Surgical Therapy for Male Infertility
- Treatment for Unknown Causes of Male Infertility
- Non-Surgical Treatment for Specific Male Infertility Conditions
Many male infertility problems can be treated without surgery.
Anejaculation
Anejaculation is when there's no semen. It's not common, but can be caused by:
- spinal cord injury
- prior surgery
- diabetes
- multiple sclerosis
- abnormalities present at birth
- other mental, emotional or unknown problems
Drugs are often tried first to treat this condition. If they fail, there are 2 next steps. Rectal probe electroejaculation (RPE, better known as electroejaculation or EEJ) is one. Penile vibratory stimulation (PVS) is the other.
Rectal probe electroejaculation is most often done under anesthesia. This is true except in men with a damaged spinal cord. RPE retrieves sperm in 90 out of 100 men who have it done. Many sperm are collected with this method. But sperm movement and shape may still lower fertility.
Penile vibratory stimulation vibrates the tip and shaft of the penis to help get a natural climax. While non-invasive, it doesn't work as well as RPE. This is especially true in severe cases.
Assisted reproductive techniques like in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI) are of great value to men with anejaculation.
Congenital Adrenal Hyperplasia (CAH)
CAH is a rare cause of male infertility. It involves flaws from birth in certain enzymes. This causes abnormal hormone production. CAH is most often diagnosed by looking for too much steroid in the blood and urine. CAH can be treated with hormone replacement.
Genital Tract Infection
Genital tract infection is rarely linked to infertility. It's only found in about 2 out of 100 men with fertility problems. In those cases, the problem is often diagnosed from a semen test. In the test, white blood cells are found. White blood cells make too much "reactive oxygen species" (ROS). This lowers the chances of sperm being able to fertilize an egg. For example, a severe infection of the epididymis and testes may cause testicular shrinking and epididymal duct blockage. The infection doesn't have to be sudden to cause problems.
Antibiotics are often given for full-blown infections. But they're not used for lesser inflammations. They can sometimes harm sperm production. Non-steroidal anti-inflammatories (such as ibuprofen) are often used instead.
Inflammation from causes other than infection can also affect fertility. For example, chronic prostatitis, in rare cases, can also block the ejaculatory ducts.
Hyperprolactinemia
Hyperprolactinemia is when the pituitary gland makes too much of the hormone prolactin. It's a factor in infertility and erectile dysfunction. Treatment depends on what's causing the increase. If medications are the cause, your health care provider may stop them. Drugs may be given to bring prolactin levels to normal. If a growth in the pituitary gland is found, you may be referred to a neurosurgeon.
Hypogonadotropic Hypogonadism
Hypogonadotropic hypogonadism is when the testicles don't make sperm due to poor stimulation by the pituitary hormones. This is due to a problem in the pituitary or hypothalamus. It's the cause of a small percentage of infertility in men. It can exist at birth ("congenital"). Or it can show up later ("acquired").
The congenital form, known also as Kallmann's syndrome, is caused by lower amounts of gonadotropin-releasing hormone (GnRH). GnRH is a hormone made by the hypothalamus. The acquired form can be triggered by other health issues such as:
- pituitary tumors
- head trauma
- anabolic steroid use.
If hypogonadotropic hypogonadism is suspected, your Doctor may want you to have an MRI. This will show a picture of your pituitary gland. You will also have a blood test to check prolactin levels. Together, an MRI and blood test can rule out pituitary tumors. If there are high levels of prolactin but no tumor on the pituitary gland, Doctor may try to lower your prolactin first. Gonadotropin replacement therapy would be the next step. During treatment, blood testosterone levels and semen will be checked. Chances for pregnancy are very good. The sperm resulting from this treatment are normal.
Immunologic infertility
Scientists first showed that some infertility cases were linked to immune system problems in the early 1950s. There has been much research since then. Though steroids (by mouth) are sometimes used to lower antisperm antibodies, this rarely works. In vitro fertilization with Intracytoplasmic Sperm Injection (ICSI) is now preferred for fertility problems caused by the immune system. This abnormality is very rare.
Retrograde ejaculation
Retrograde ejaculation, semen flowing back instead of going out the penis, has many causes. It can be caused by:
- prostate or bladder surgeries
- diabetes
- spinal cord injury
- anti-depressants
- certain anti-hypertensives
- medications used to treat prostate enlargement (BPH)
Retrograde ejaculation is found by checking your urine for sperm. This is done under a microscope right after ejaculation. Drugs can be used to correct retrograde ejaculation.
If medications don't work and you need assisted reproductive techniques (ARTs), your Doctor may try to collect sperm from your bladder after ejaculation.
Surgical Therapy for Male Infertility
Varicocele Treatments
Varicoceles can be fixed with the surgery called varicocelectomy. Fixing these swollen veins helps sperm movement, numbers, and structure.
What are Varicoceles?
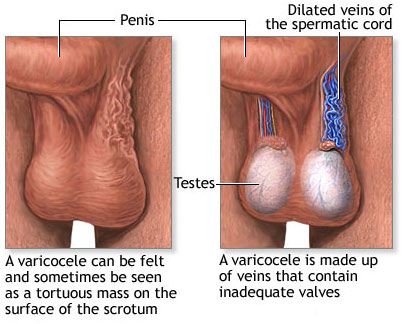
A varicocele is when veins become enlarged inside your scrotum (the pouch of skin that holds your testicles). These veins are called the pampiniform plexus. Ten to 15 of every 100 males have a varicocele. It is like getting a varicose vein in your leg.
What Happens Normally?
The male reproductive system makes, stores, and moves sperm. The scrotum is the sac of skin that holds the testicles (testes). Sperm and the hormone testosterone are made in the testicles. Sperm mature while moving through a coiled tube (the epididymis) behind each testicle.
Sperm travel to the prostate from each epididymis using a tube called the vas deferens. When you ejaculate, seminal fluid mixes with sperm in the prostate to form semen. The semen travels through the urethra and comes out the end of your penis.
The spermatic cord holds the vas deferens and the testicular artery, which brings blood to the testicle. It also houses the pampiniform plexus, a group of connected veins that drains the blood from the testicles. The pampiniform plexus cools blood in the testicular artery before it enters the testicles. This helps keep it at the temperature needed to make sperm.
What are Varicoceles?
Varicoceles are when the pampiniform plexus veins in the scrotum become enlarged. These veins are like varicose veins in the leg. Varicoceles form during puberty, and can grow larger and easier to notice over time. Varicoceles are more common on the left side of the scrotum. This is because the male anatomy isn't the same on both sides. Varicoceles can exist on both sides at the same time, but this is rare. About 10 to 15 boys out of 100 have a varicocele.
Most of the time, varicoceles cause no problems and are harmless. Less often varicoceles can cause pain, problems fathering a child, or 1 testicle to grow slower or shrink.
What are Signs of a Varicocele?
Most males with a varicocele have no symptoms. But varicoceles are a concern for many reasons. Some may cause infertility (problems fathering a child) and slow growth of the left testicle during puberty. Varicoceles may be the cause of fertility problems in about 4 out 0f 10 men who have problems fathering their first child. They may also be the cause of fertility problems in about 8 out of 10 men who have problems fathering a child after their first.
What Can Cause Varicoceles?
Many causes of varicoceles have been offered. The valves in the veins may not work well (or may be missing). If blood flow is sluggish, blood may pool in the veins. Also, the larger veins moving from the testicles towards the heart are connected differently on the left and right side. So more pressure is needed on the left side to keep blood flowing through the veins towards the heart. If blood flows backwards or pools in the veins, that can cause them to swell. Rarely, swollen lymph nodes or other abnormal masses behind the abdomen block blood flow. This can lead to sudden swelling of the scrotal veins. This is often painful.
Are Varicoceles Common?
About 15 out of 100 men have varicoceles. It's hard to predict which of these 15 will have fertility problems caused by their varicocele. But about 4 in every 10 men tested for fertility problems have a varicocele and decreased sperm movement. There's no link with other defects, race, place of birth, or ethnic group. Although varicoceles are often found in men tested for infertility, 8 out of 10 men who have a varicocele don't have fertility problems.
How are Varicoceles Diagnosed?
Varicoceles are found through self-exam of the scrotum or during a routine doctor’s exam. They’ve been described as a “bag of worms” because of how they look and feel.Urologists often check for varicoceles with the patient standing.
Your urologist may order a scrotal ultrasound test. Signs of varicoceles on ultrasound are veins that are wider than 3 millimeters with blood flowing the wrong way during the Valsalva maneuver. The ultrasound can also show the size of the testicles. These are useful in deciding how to treat teenagers.
How are Varicoceles Treated?
Often, varicoceles are not treated. Treatment is offered for males who have:
- fertility problems (problems fathering a child)
- pain
- the left testicle growing more slowly than the right
- Boys with a smaller left testicle are thought to have a higher risk for fertility problems when they get older.
There are no drugs to treat or prevent varicoceles. But pain killers (such as acetaminophen or ibuprofen) may help with pain.
When needed, surgery is the main form of treatment. Embolization (briefly blocking the veins) is a non-surgical treatment option.
Surgery
There are many ways to do varicocele surgery. All involve blocking the blood flow in the pampiniform plexus veins.
Open Surgery
Open surgery repair is done through a single 1 inch cut. The surgeon may use a magnifying glass or operating microscope to see small veins. The surgery can be done under local or general anesthesia.
Laparoscopic Surgery
Laparoscopic surgery is done through thin tubes put into your body through a small cut. The surgeon uses a special camera to see inside your body. Laparoscopic surgery is done under general anesthesia.
Surgery Results
Since surgeons have started using smaller cuts through the muscle for open surgery, healing time and pain are about the same with open and laparoscopic surgery. Problems after either surgery are rare.
Problems include:
- varicocele remaining (persistence) or coming back (recurrence)
- fluid forming around the testicle (hydrocele)
- injury to the testicular artery
There is a small chance surgery won't correct the problem. Persistence or recurrence of the varicocele happens in fewer than 1 of 10 patients who have surgery. Open surgery done with magnification has a low persistence rate or chance of varicocele coming back.Most of the time, patients return to normal activities after 2 days with little pain.
Percutaneous Embolization
Embolization is done by a radiologist. A special tube is put into a vein in either the groin or neck. An X-ray is used to check the enlarged pampiniform plexus veins. Then coils or balloons are opened through the tube to block the veins. This halts the blood flow in the pampiniform plexus veins and the varicocele shrinks. Percutaneous embolization is most often done with general anesthesia. It often takes several hours.
Some problems are:
- varicocele remaining (persistence) or coming back (recurrence)
- the coil moving from where it was placed
- a chance of infection where the tube was placed
This method isn't used at most centers.
Azoospermia Treatments
If your semen lacks sperm (azoospermia) because of a blockage, there are many surgical choices.
Microsurgical Vasovasostomy
Vasovasostomy is used to undo a vasectomy. It uses microsurgery to join the 2 cut parts of the vas deferens in each testicle.
Vasoepididymostomy
Vasoepididymostomy joins the upper end of the vas deferens to the epididymis. It's the most common microsurgical method to treat epididymal blocks.
Transurethral Resection of the Ejaculatory Duct (TURED)
Ejaculatory duct blockage can be treated surgically. A cystoscope is passed into the urethra (the tube inside the penis) and a small incision is made in the ejaculatory duct. This gets sperm into the semen in about 65 out of 100 men. But there can be problems. Blockages could come back. Incontinence and retrograde ejaculation from bladder damage are other possible but rare problems. Also, only 1 in 4 couples get pregnant naturally after this treatment.
Treatment for Unknown Causes of Male Infertility
Sometimes it's hard to tell the cause of male infertility. This is called "non-specific" or "idiopathic" male infertility. Your health care provider may uses experience to help figure out what works. This is called "empiric therapy." Because infertility problems are often due to hormones, empiric therapy might balance hormone levels. It's not easy to tell how well empiric treatments will work. Each case is different.
Assisted Reproductive Techniques
If infertility treatment fails or isn't available, there are ways to get pregnant without sex. These methods are called assisted reproductive techniques (ARTs). Based on the specific type of infertility and the cause, your health care provider may suggest:
Intrauterine Insemination (IUI)
For IUI, your health care provider places the sperm into the female partner's uterus through a tube. IUI is often good for low sperm count and movement problems, retrograde ejaculation, and other causes of infertility.
In Vitro Fertilization (IVF)
IVF is when the egg of a female partner or donor is joined with sperm in a lab Petri dish. For IVF, the ovaries must be overly stimulated. This is often done with drugs. It allows many mature eggs to be retrieved. After 3 to 5 days of growth, the fertilized egg (embryo) is put back into the uterus. IVF is used mostly for women with blocked fallopian tubes. But it's being used more and more in cases where the man has very severe and untreatable oligospermia (low sperm count).
Intracytoplasmic Sperm Injection (ICSI)
ICSI is a variation of IVF. It has revolutionized treatment of severe male infertility. It lets couples thought infertile get pregnant. A single sperm is injected into the egg with a tiny needle. Once the egg is fertilized, it's put in the female partner's uterus. Your Doctor may use ICSI if you have very poor semen quality. It is also used if you have no sperm in the semen caused by a block or testicular failure that can't be fixed. Sperm may also be taken from the testicles or epididymis by surgery for this method.
Sperm Retrieval for ART
Many microsurgical methods can remove sperm blocked by obstructive azoospermia (no sperm). The goal is to get the best quality and number of cells. This is done while trying not to harm the reproductive tract. These methods include:
Testicular Sperm Extraction (TESE)
This is a common technique used to diagnose the cause of azoospermia. It also gets enough tissue for sperm extraction. The sperm taken from the testicle can be used fresh or frozen ("cryopreserved"). One or many small biopsies are done, often in the office.
Testicular Fine Needle Aspiration (TFNA)
TFNA was first used to diagnose azoospermia. It is now sometimes used to collect sperm from the testicles. A needle and syringe puncture the scrotal skin to pull sperm from the testicle.
Percutaneous Epididymal Sperm Aspiration (PESA)
PESA, like TFNA, can be done many times at low cost. There is no surgical cut. More urologists can do it because it doesn't call for a high-powered microscope. PESA is done under local or general anesthesia. The urologist sticks a needle attached to a syringe into the epididymis. Then he or she gently withdraws fluid. Sperm may not always be gotten this way. You may still need open surgery.
Microsurgical Epididymal Sperm Aspiration (MESA)
With MESA, sperm are also retrieved from the epididymal tubes. This method uses a surgical microscope. MESA yields high amounts of motile sperm. They can be frozen and thawed later for IVF treatments. This method limits harm to the epididymis. It keeps blood out of the fluid. Even though MESA calls for general anesthesia and microsurgical skill, it has a lower problem rate. It's also able to collect larger numbers of sperm with better motility for banking.
